Everyone deserves to be looked in the face and understood—to the best of our abilities
Being the vulnerable human beings we all are, we assume things about chronic conditions such as hepatitis C. We assume it is a disease of Baby Boomers, of people who use needles. Ultimately, it’s something that won’t happen to us.
Because of such myths, many patients fall through the cracks. As health care providers, nurses, case managers, or whatever the title, we think of ourselves as “community educators.” We talk and talk while patients look at us with wide eyes, nodding hesitantly. Are we really listening and processing their stories? What can we learn from them?
Hepatitis C in brief
As an infection of the liver that is caused by a virus transmitted through contaminated blood, hepatitis C (HCV), if left untreated, can lead to serious, and oftentimes irreversible, liver damage. Until a few years ago, hepatitis C treatment required weekly injections and oral medications that many people living with HCV could not take because of other health problems or unacceptable side effects. But with the bloom of drug options, chronic HCV is now promisingly curable with oral medications that are taken every day for two to three months with minimal side effects, if any.
Access to a cure, however, is still elusive.
Although 30% of people self-clear the virus spontaneously and antiviral medications are 98% effective in curing chronic infections, access to testing and treatment remain staggered. The World Health Organization (WHO) estimates that 71 million people have chronic HCV globally, with only 19% aware of their diagnosis. The U.S. Centers for Disease Control and Prevention (CDC) estimated 2.4 million people were living with HCV in the U.S. in 2014, and that the death toll associated with HCV reached 19,659. Because this figure was based on death certificates, which often underreport HCV, it is likely that the death toll is actually higher. These estimates reflect a mortality rate that surpasses the total number of deaths attributed to 60 other infectious diseases combined, including HIV, pneumococcal complications, and tuberculosis. These deaths are a testament to our systemic mistakes in the proper testing and swift treatment of HCV.
Although badly needed, HCV treatments are very expensive, costing about $84,000 for a full 12-course treatment of the latest drug. In one analysis, if all 300,000 Medicare patients projected to be diagnosed by 2015 were to seek treatment with the latest drugs after screening, the total expenditure could exceed $25 billion. That does not include the cost of lab appointments, doctor visits, and other fees. For those that are not eligible for insurance this is an impossible amount of money to pay.
Insurance no guarantee
These cost barriers are not altogether eliminated for those who are insured. Janice Brockman was diagnosed with HCV during a 2016 hospital visit. She was surprised by the news, but was immediately informed there was an effective treatment and given a referral for a specialist at a prominent Chicago hospital.
After a few months of follow-up visits and consultations, she was told she was not eligible for treatment because her insurance, an Illinois managed Medicaid plan, would not pay for it.
This story represents one of the primary barriers to HCV treatment in the U.S., the restrictions that plague access and often result in patients developing permanent liver damage before they receive treatment.
In 2019, these restrictions were lifted in Illinois as a result of legal advocates filing a lawsuit against the state, but prior to this point Medicaid plans would not pay for treatment unless a person completed additional testing, urine drug screens, and showed high levels of liver scarring and inflammation. Hepatitis C-related liver damage is typically a slow process, and these restrictions created systems where patients would wait for years to develop enough damage so they could qualify for treatment, leaving them with irreversible liver scarring that increased their risk of liver cancer. This is what happened to Brockman.
‘I couldn’t attend family functions’
After three attempts to get treatment from three different care centers, Brockman started her medications in 2020 through our clinic, Howard Brown Health, in Chicago. Shortly into her first round of treatment, she started showing significant side effects and was sent to the hospital, where she was discovered to have a cancerous tumor attached to her liver. The tumor caused the side effects, and having completed an ultrasound of her liver a few months prior, it was a decidedly recent development.
Janice Brockman and Eddie Mendez.
Brockman completed HCV treatment after seeing an oncologist, and today she is now cured of HCV and her cancer is in remission. However, this cancer was likely avoidable if she had been provided treatment soon after her HCV diagnosis. She also suffered through years of HCV-related symptoms that significantly impaired her life, including extreme fatigue and anemia, for which she was regularly hospitalized to receive blood transfusions.
Now that she’s cured she realizes just how severely the HCV had affected her. “I feel incredible now, after years of feeling horrible. I couldn’t attend family functions, parties, anything. I missed out on so much because all I wanted to do was lay up in bed.”
Although Illinois lifted its Medicaid restrictions, the same restrictions still exist in many states and represent a huge disparity in who is able to access treatment, and sadly, who is more likely to die of liver disease.
A special collaboration
The many barriers affecting access to HCV treatment and cure are of special concern for people of immigrant experience. At Howard Brown, we strive to reduce the common language and insurance barriers experienced by this community. In part we’ve done this by partnering with Mongolian community representatives to better support Mongolian speakers specifically, because of their high rates of HCV and HBV.
Bayarmaa Shravdorj found she was living with HCV when she came in for a screening. Because HCV frequently shows no symptoms, she was unaware of her status, but unfortunately, she was painfully aware of what it meant. “I had some minor information about it from family and friends. My dad and younger siblings died from hepatitis viruses.”
Shravdorj’s loss is tragic, yet common. The majority of our Mongolian patients report the death of at least one immediate family member to hepatitis-related liver disease. It is because of this that the community is engaged in finding resources. However, many care facilities can’t accommodate Mongolian speakers or treat individuals without insurance, and people have a hard time even getting screened.
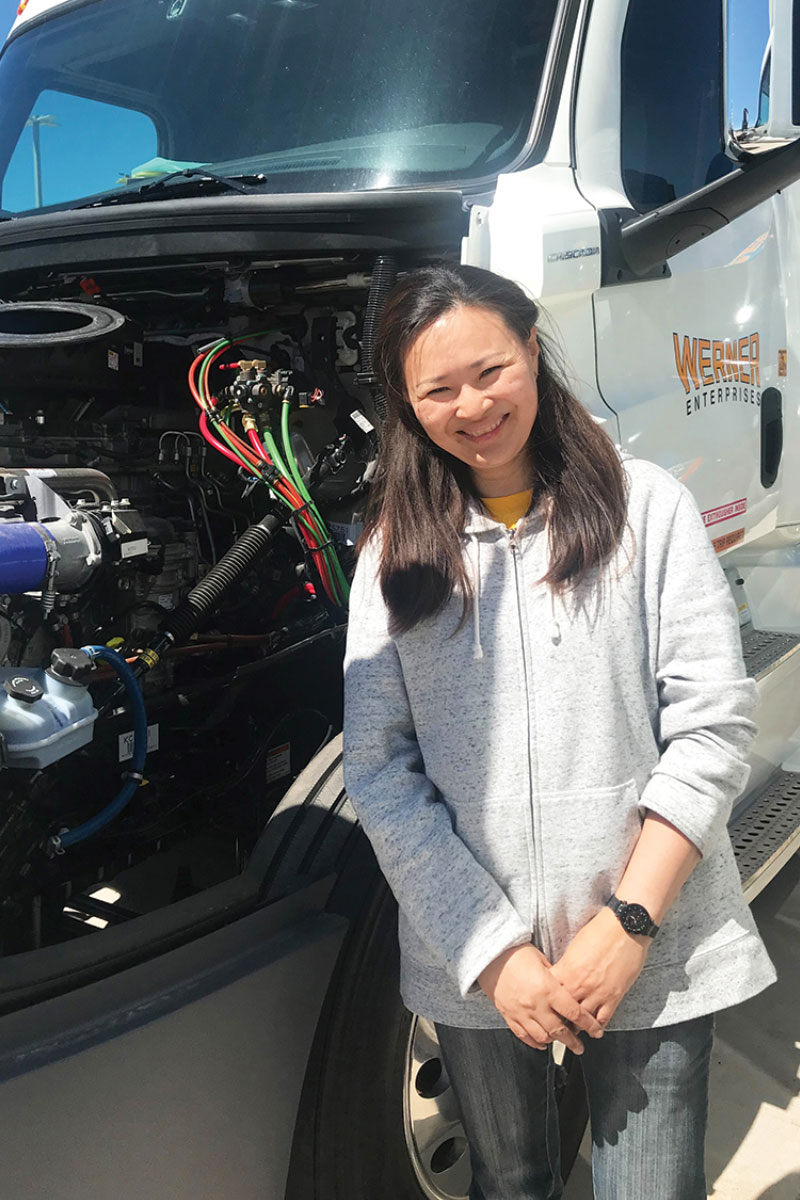
On the road: Bayarmaa Shravdorj with her rig.
Fortunately, we have been able to access medications for this group by using pharmaceutical assistance programs, which is how we were able to offer treatment immediately to Shravdorj.
“When I found out I had hepatitis C at Howard Brown Health ... I felt overwhelmed,” she said. “I didn’t know what to do, but they told me they offered treatment and I embraced it with open arms and was very happy. I told my family I had hepatitis C and they were very supportive. Howard Brown Health told me it was fully treatable and they were very supportive too.”
HIV/HCV co-infection
As for people living with HIV (PLWH), they are at a high risk for not only contracting HCV but also developing liver damage at a faster rate. The Department of Health and Human Services (DHHS) reports that of the PLWH in the U.S., about a quarter are co-infected with HCV, and those who are co-infected are over three times more likely to develop liver disease, liver failure, and liver-related death. For injection drug users living with HIV, the rate of HCV co-infection is about 75%.
Although we know the risk of co-infection, we still lack sufficient HCV screening among PLWH. At an STI clinic in Miami, only about 15% of participants were screened for HCV while 83% had been screened for HIV; and 98% of the participants had been previously screened for HIV as well.
For our co-infected community, universal screening and quick administration of treatment are particularly necessary. All PLWH should be screened for HCV upon entry into primary care, and providers should establish a testing routine based on the risk factors patients present.
Incarceration
Around the world, incarcerated people experience a higher incidence of HCV than the general population. However, they have routinely struggled to access medications and medical treatment.
The primary risk factor associated with this infection rate is injection drug use, followed by illicit tattooing, sexual behavior, and to a lesser extent, sharing of toiletries. People using drugs inside the prison system do not have access to sterile use supplies, contributing to the high transmission rate via injection use.
Of the participants Howard Brown has treated, multiple people have identified that their most likely exposures to HCV were during their time in prison, and all have attested to the lack of treatment available. The reasons reported for how and why our formerly incarcerated patients did not receive adequate HCV care vary. Some reported that testing for HCV was not available until they were about to leave or had just left prison. Other factors included lack of general access to medical care, being told they are not sick enough, and denial of medication requests due to the length of their sentence.
All of these have the same harmful effect: patients endure an unnecessary disease progression, and other inmates’ risk of HCV exposure is increased.
Injection drug use
In the midst of an opioid epidemic, we must acknowledge the most considerable contributor to HCV transmission in the U.S., injection drug use. In 2018 the CDC HCV Surveillance Report showed that a majority of people are unable to identify how they were exposed, but of those who can, 72% report current or past injection drug use.
The opioid crisis has especially affected a younger age group, demonstrated by a 23% increase in new infections among people aged 20–39. In the city of Chicago alone, the infection rate among people who were born after 1986 increased by 288% between 2013–2017. Many state Medicaid systems require urine drug screens and six months of sobriety to be eligible for HCV treatment. People using drugs and alcohol are more likely to experience a lack of stability in housing and income, making strict eligibility criteria difficult to meet. There’s also been a trend of hospitals and clinical practices imposing their own sobriety measures in pursuit of treating patients who they believe will be more successful.
It is important to note that there is no immunity gained by HCV treatment. We can cure the infection a person has, but they will not be immune moving forward and require education on how to avoid re-infection after treatment. This re-infection principle is the primary argument for not treating people who actively use drugs, in addition to the assumptions made by clinicians about their ability to engage in medical care.
However, current national HCV treatment guidelines recommend the treatment of patients using drugs. Even with the potential risk of re-infection, by treating everyone with HCV we are lowering the risk of community transmission and ensuring patients do not develop liver disease.
Brockman with Alaa Wasfi
I feel incredible now, after years of feeling horrible. I couldn’t attend family functions, parties, anything. I missed out on so much because all I wanted to do was lay up in bed.
Our program
Effective HCV treatment requires an acceptance of all clients, and a multidisciplinary method of support. At Howard Brown we strive to maintain accessibility by offering treatment to everyone who comes in regardless of insurance, documentation, active drug and alcohol use, housing stability, or lapses in engagement. There is a long-established national trend of treatment denial based on these factors. If we have any hope of eliminating HCV, it’s crucial to treat all patients. In order to see that all clients achieve a cure, our team consists of a pharmacist, nurse, and case managers who work to support clinicians in treating people with HCV, and assist those individuals in identifying and addressing barriers to treatment. By employing harm reduction, we adjust care plans to fit each person’s feedback about what they need to make the treatment a success. We focus on educating clients about HCV and the treatment process so they can make informed decisions about their care.
One client, Eddie Mendez, says it best:
“Have a good doctor, a great doctor. I wish [my previous provider] would have pushed me more, but I understand why he didn’t. He completely left it in my court. And get a great team to help you. Be involved. Don’t be ashamed. It’s not a killer anymore. I feel so lucky. I’ve seen what it’s done to people. It’s testable and it’s curable and that’s pretty awesome.”
Alaa Wasfi, RN, BSN (she/they) is a primary care and sexual health Registered Nurse at Howard Brown Health since 2016. She presented on “Increasing HCV Treatment Through Reducing Stigma in an LGBTQ Health Setting” at the National Harm Reduction Conference, New Orleans 2018. Alaa was born and raised in Iraq. Her life’s motto: “Everyone deserves to be looked in the face and understood—to the best of our abilities.”
Sam Forsythe (she/her/hers) is an HCV Community Engagement Specialist at Howard Brown Health. She began working in HIV case management services for women of all ages and youth in 2015 and transitioned to HCV case management and outreach in 2018 where she has focused on engaging groups that experience significant barriers to hepatitis C treatment, including people with active use or a history of drug use, those of immigrant experience, and people without documentation.
Howard Brown Health’s HCV team provides hepatitis C treatment and education to all individuals regardless of past denials, substance use, insurance, or documentation status, and aims to provide multidisciplinary support from diagnosis to cure. Howard Brown’s mission is to eliminate the disparities in healthcare experienced by lesbian, gay, bisexual, and transgender people through research, education, and the provision of services that promote health and wellness.